Obsessive Compulsive Disorder (OCD) Formulation
Download or send
Related resources
Tags
Languages this resource is available in
Problems this resource might be used to address
Techniques associated with this resource
Mechanisms associated with this resource
Introduction & Theoretical Background
The essential insight of the cognitive behavioral model of obsessive compulsive disorder (OCD) is that it is the client’s interpretation of the intrusion which drive the distress and maladaptive responses (Salkovskis, Forrester & Richards, 1998). Intrusive thoughts, images, urges, and doubts are very common and entirely normal (Purdon and Clark, 1993, 1994): what gives intrusions their emotional power in OCD is the meaning that clients assign to them. Individuals with OCD commonly interpret the occurrence or content of their intrusions as:
- Meaning something bad about them and/or that something bad will happen, and
- Believing that they are personally responsible for preventing harm to themselves and/or others
Interpreting intrusions through the lens of responsibility has a number of effects including: increased discomfort, increased focus of attention on the intrusions, increased accessibility of the intrusions, active attempts to reduce the intrusions, and attempts to decrease or discharge the responsibility that the individual perceives is associated with them. Although these efforts can lead to short-term reductions in anxiety, in the long-term they increase preoccupation with the intrusive thoughts and maintain the pattern of responses to them.
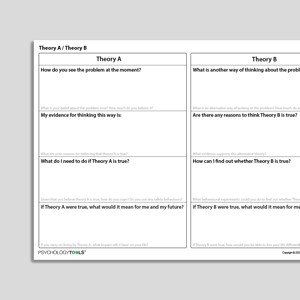
An important treatment implication of the cognitive behavioral model of OCD is that clinicians can work at the level of the meaning of the intrusion. This can be contrasted with traditional exposure and response prevention, which can be framed as an intervention at the level of the compulsion or neutralizing behavior. Clients can be helped to develop an alternative, less-threatening, interpretation of what the intrusions mean (theory b), and then to test this alternative through a process of information-gathering which might include symptom monitoring, behavioral experiments, and exposure exercises. The Obsessive Compulsive Disorder (OCD) Formulation worksheet is a case conceptualization tool for cognitive behavioral therapists.
Therapist Guidance
This worksheet is designed as a case conceptualization tool for therapists. If it is used with clients it can help to structure a discussion about how the client’s experiences and reactions interact. Case conceptualization is considered to be most effective when it is collaborative exploration of a client’s difficulties rather than presented as a ‘completed solution’ (Kuyken, Padesky, Dudley, 2011). If the worksheet is used in session with a clients, it is best introduced as a tentative tool for exploration.
The therapist might introduce it by saying “some people’s OCD responses fit the pattern on this diagram. I wonder if we could we explore some of your thoughts, feelings, and reactions and see what kind of pattern they follow?”.
- Ask the client to think of a recent time when they experienced an intrusion
- Help the client to focus on the meaning of the intrusion: “What does it say about you that you had this intrusion / thought / image / doubt / urge?” “What would other people think of you if they knew you had this thought?” “How responsible do you feel for preventing this event from happening?” “If other people knew you had this thought how responsible would they think you are for preventing [negative outcome] from happening?”
- Help the client to describe their responses to interpreting the intrusion in this way: “What do you do to cope?” “What do you do to prevent the worst from happening?” “What do you pay extra attention to or look out for?” “What do you feel when you think about things in this way?”
- Explore the consequences of the client’s reactions and consider whether any of these reactions might act to reinforce the cycle. A common pattern to look for is that reactions lead to short-term improvements (e.g. feeling safer) but either no change to, or a worsening of, the sequence in the long-term.
References And Further Reading
- Kuyken, W., Padesky, C. A., & Dudley, R. (2011). Collaborative case conceptualization: Working effectively with clients in cognitive-behavioral therapy. Guilford Press.
- Purdon, C., & Clark, D. A. (1993). Obsessive intrusive thoughts in nonclinical subjects. Part I. Content and relation with depressive, anxious and obsessional symptoms. Behaviour Research and Therapy, 31(8), 713-720.
- Purdon, C., & Clark, D. A. (1994). Obsessive intrusive thoughts in nonclinical subjects. Part II. Cognitive appraisal, emotional response and thought control strategies. Behaviour Research and Therapy, 32(4), 403-410.
- Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioural approach to understanding obsessional thinking. The British Journal of Psychiatry, 173(S35), 53-63.