Free Guide (PDF)
A free psychoeducational guide. Typically containing elements of skills development.
A guide addressing written for people experiencing symptoms of post-traumatic stress disorder (PTSD) following experiences of critical illness or intensive care.

A free psychoeducational guide. Typically containing elements of skills development.
To use this feature you must be signed in to an active account on the Advanced or Complete plans.
This guide explores the psychological challenges arising from critical illness and ICU experiences, particularly focusing on PTSD symptoms. It is an essential resource for mental health and medical professionals aiming to support patients recovering from traumatic medical experiences.
Given the impact of recent global health crises, understanding and addressing PTSD related to critical care experiences is more important than ever. This guide offers practical information to aid recovery and promote mental health.
Understanding PTSD in the context of critical illness is vital for providing effective care.
People experiencing symptoms post-ICU.
Manifesting after prolonged medical care.
Concerns about medical recurrences or future illnesses.
Use the guide to educate about the psychological impacts of ICU care.
Help patients identify triggers and symptoms of PTSD.
Assess for PTSD using structured tools mentioned in the guide.
Implement therapeutic tasks and provide support based on guide recommendations.
Work with medical staff to ensure a holistic approach to patient care.
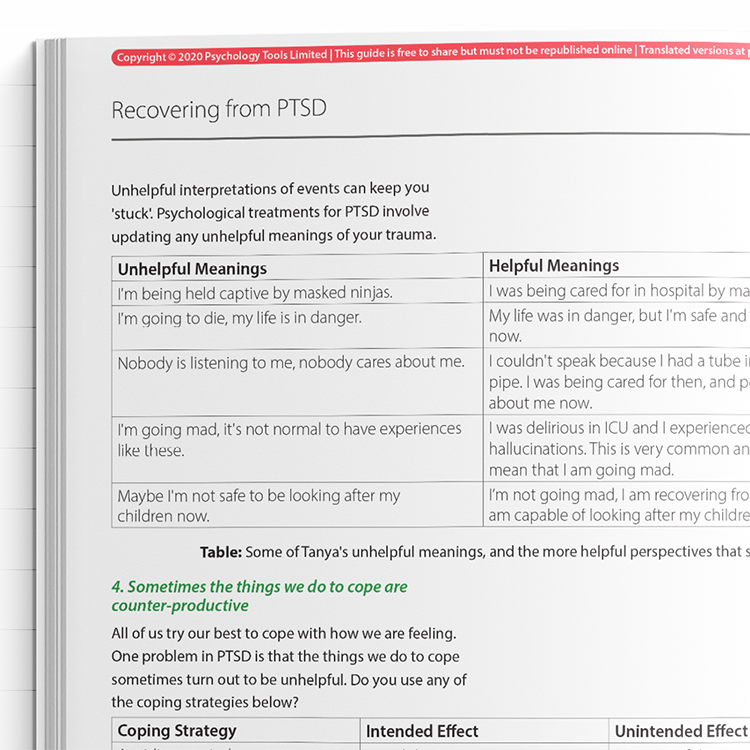
The guide utilizes cognitive behavioral therapy (CBT) principles and eye movement desensitization and reprocessing (EMDR) for understanding and treating PTSD. It explains the psychological impact of ICU stays, including the role of delirium and trauma memory processing. It emphasizes the importance of meaning-making and coping strategies, highlighting common maladaptive beliefs and how they can perpetuate PTSD symptoms. Therapists are encouraged to help patients process fragmented trauma memories and explore site visits or patient records to aid recovery.
Survivors of critical illness and intensive care often experience significant psychological distress after discharge, including symptoms consistent with post-traumatic stress disorder (PTSD). ICU-related PTSD is now recognized as a common consequence of intensive care, affecting approximately 1 in 5 patients (Righy et al., 2019). The development of PTSD in this context can be linked to factors such as delirium, invasive procedures, perceived threat to life, sensory deprivation, and frightening hallucinations (Cavallazzi et al., 2012).
This guide draws primarily on cognitive behavioral therapy (CBT) and eye movement desensitization andreprocessing (EMDR) frameworks, both of which are evidence-based approaches for treating PTSD. In line with the cognitive model of PTSD (Ehlers & Clark, 2000), individuals who survive ICU may struggle with fragmented trauma memories, negative appraisals (e.g., “I was helpless” or “I’m permanently damaged”), and avoidance behaviors that prevent recovery.
ICU survivors often experience disorientation and memory gaps due to sedation and delirium, making trauma processing more complex. Maladaptive interpretations of these unusual sensory experiences (e.g., hallucinations or delusions) can maintain hyperarousal and intrusive symptoms. The guide emphasizes meaning-making, reconstruction of trauma narratives, and, where appropriate, site visits or reviewing medical records to fill in memory gaps—strategies supported by trauma-focused CBT literature (Murray et al., 2020).
By supporting clients in understanding their reactions and connecting these to trauma responses—not mental deterioration—therapists can help reduce shame, foster psychological integration, and promote recovery.

Just enter your name and email address, and we'll send you [Free Guide] Critical Illness Intensive Care And Post-Traumatic Stress Disorder (PTSD) (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy