Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
A licensed copy of Harvey's (2002) cognitive behavioral model of insomnia which describes a framework to address key components of this disorder.
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
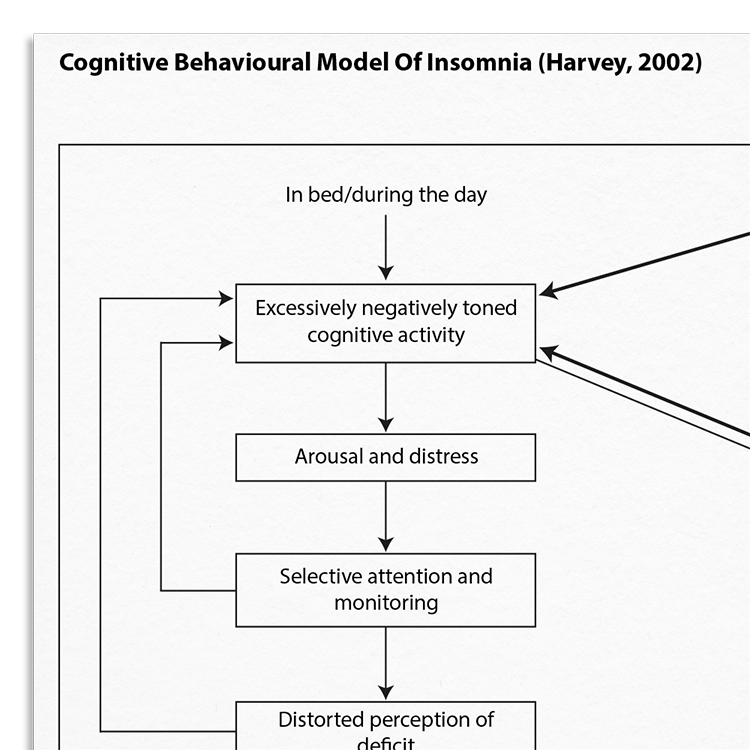
Insomnia is a highly prevalent sleep disorder characterized by difficulty initiating or maintaining sleep, or having non-restorative sleep for at least one month. Sleep problems are extremely common in people who suffer from mental health problems and there is increasing evidence that disturbed sleep can be a causal factor for many mental health difficulties. Harvey’s (2002) cognitive model of insomnia suggests that excessive worrying about a lack of sleep triggers autonomic arousal and emotional distress. This increased arousal leads to selective attention towards and increased monitoring of sleep-related threat cues, culminating in a biased perception of the sleep-related deficit.
The Cognitive Behavioral Model Of Insomnia can be used to conceptualize your client's insomnia. It is a useful framework for identifying safety behaviors and unhelpful beliefs about sleep or worry, both of which Harvey highlights as key exacerbating factors. This model proposes that cognitive processes contribute to the maintenance of insomnia, irrespective of whether the original cause was psychiatric, circadian, medical, or drug-induced.
Understanding the underpinnings of insomnia is important for effective intervention. This resource helps clinicians:
Ideal for mental health professionals working with clients experiencing insomnia.
Understand more about the cognitive behavioral model of insomnia.
Use the model as a template to organize your case formulations.
Use your knowledge of the model to explain maintenance processes to clients.
Engage clients in discussions about their beliefs and behaviors.
Customize interventions based on individual maintenance mechanisms.
Use in supervision to discuss case conceptualizations and treatment plans.
Insomnia is one of the most prevalent sleep disorders, affecting around 10% of the population. There is a sound evidence base showing that it is an exacerbating factor many in psychological disorders, and it is frequently reported by people struggling with anxiety and depression (although it is not a primary symptom). Symptoms of insomnia may include struggling to fall asleep or initiate sleep, taking a long time to fall asleep (prolonged sleep onset time), waking repeatedly in the night, sleeping for only short periods in the night, and waking early and being unable to get back to sleep.
Harvey’s Cognitive Model Of Insomnia (2002) highlights the importance of negative cognitions related to sleep. These occur both at night-time, when the client is trying to fall asleep or finds themselves awake, and during the day, when they are preoccupied with how poor sleep may have affected them, or how they are going to sleep that night. Key components of this model include excessively negative cognitive activity, arousal and distress, selective attention and monitoring, and distorted perception of deficit.

Just enter your name and email address, and we'll send you Cognitive Behavioral Model Of Insomnia (Harvey, 2002) (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy