Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
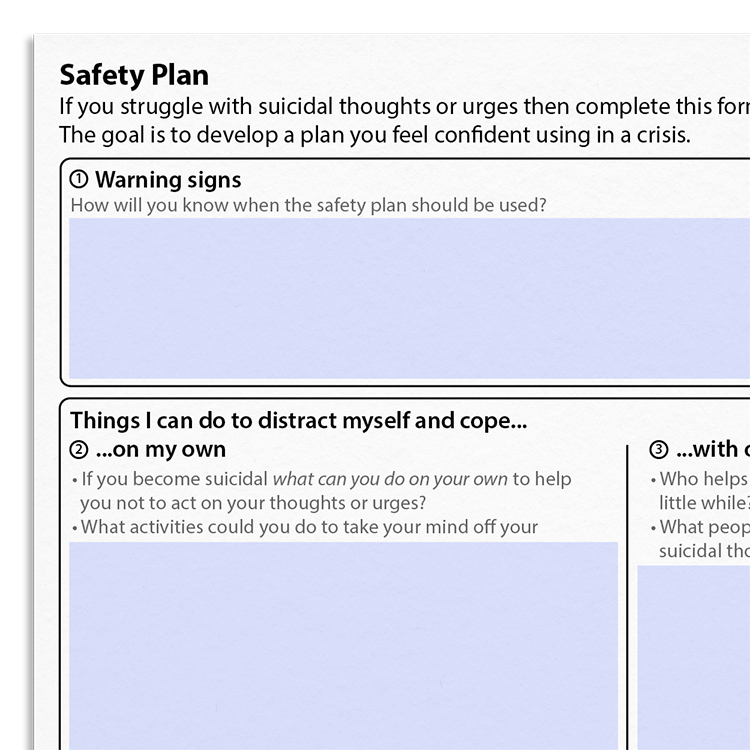
Client version
Includes client-friendly guidance. Downloads are in Fillable PDF format where appropriate.
Editable version (PPT)
An editable Microsoft PowerPoint version of the resource.
Editable version (DOC)
An editable Microsoft Word version of the resource.