Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
A licensed copy of Hunter and colleagues (2003) cognitive model of depersonalization.

Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
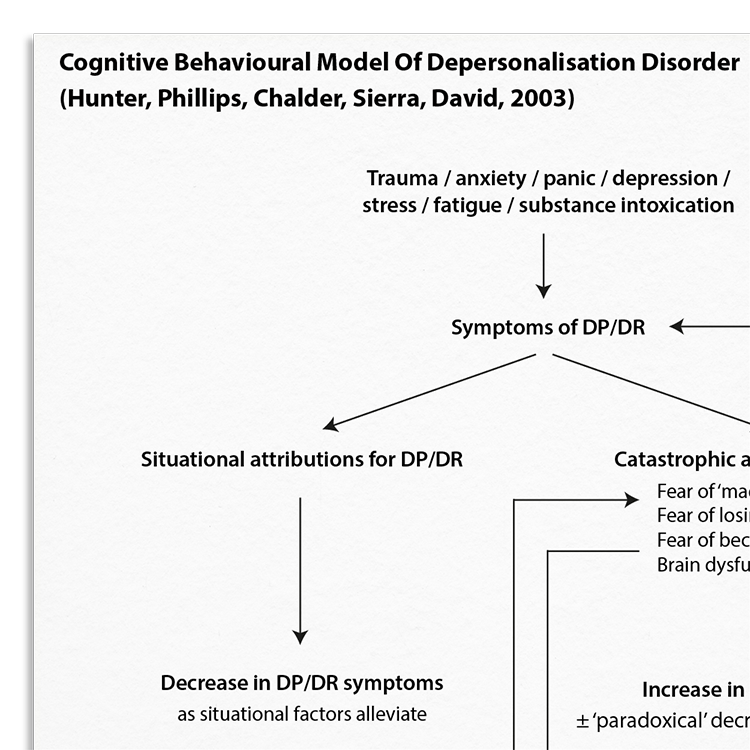
Depersonalization is an experience where an individual feels a sense of detachment from themselves, or estrangement from their perceptions, actions, and feelings. It can be accompanied by derealization, where the external world appears unfamiliar or less real. Both can be transient experiences, are experienced by up to 70% of non-clinical populations, and are often associated with fatigue, stress, or drug use. Depersonalization disorder (DPD) is diagnosed when symptoms of depersonalization and derealization are experienced chronically and cause significant distress and impairment. It can occur in the absence of other conditions or as a comorbid condition. The Cognitive Behavioral Model of Depersonalization information handout reproduces a cognitive model of DPD proposed by Hunter, Phillips, Chalder, Sierra, & David (2003).
Understanding the key underpinnings of depersonalization is important for effective intervention.
Ideal for therapists working with individuals affected by depersonalization.
Understand more about the cognitive model of personalization.
Use the model as a template to organize your case formulations.
Use your knowledge of the model to explain maintenance processes to clients.
Engage clients in discussions about their beliefs and behaviors.
Customize interventions based on individual maintenance mechanisms.
Use in supervision to discuss case conceptualizations and treatment plans.
Depersonalization disorder (DPD) is a chronic condition in which an individual experiences frequent or unremitting detachment from themselves, disrupting the normally integrated sense of self. Critically, people experiencing DPD are not delusional: they retain insight, and their awareness of the disjunction between the observing self and the embodied self causes significant distress (Hunger et al, 2003; Medford et al, 2005). Core symptoms of DPD include depersonalization (DP), derealization (DR), and cognitive changes (e.g., impaired concentration, a changed perception of time, an empty mind or racing thoughts, or difficulty processing new information).
Hunter, Phillips, Chalder, Sierra and David (2003) proposed a cognitive model to account for the maintenance of DPD, which suggests that common, transient symptoms of DP/DR (typically experienced during times of stress or threat) are catastrophically misinterpreted as signs of deteriorating or damaged mental health. This leads to feelings of anxiety and associated physiological reactions, which may then exacerbate the symptoms of DP/DR. Similar to other anxiety disorders, they propose that the cycle is maintained by avoidance, safety behaviors and heightened symptom monitoring and self-focused attention.

Just enter your name and email address, and we'll send you Cognitive Behavioral Model Of Depersonalization (Hunter, Phillips, Chalder, Sierra, David, 2003) (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy