Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
A licensed copy of the Whalley & Cane (2017) cognitive behavioral model of persistent postural-perceptual dizziness which describes a framework to address the core components and symptoms of PPPD.
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
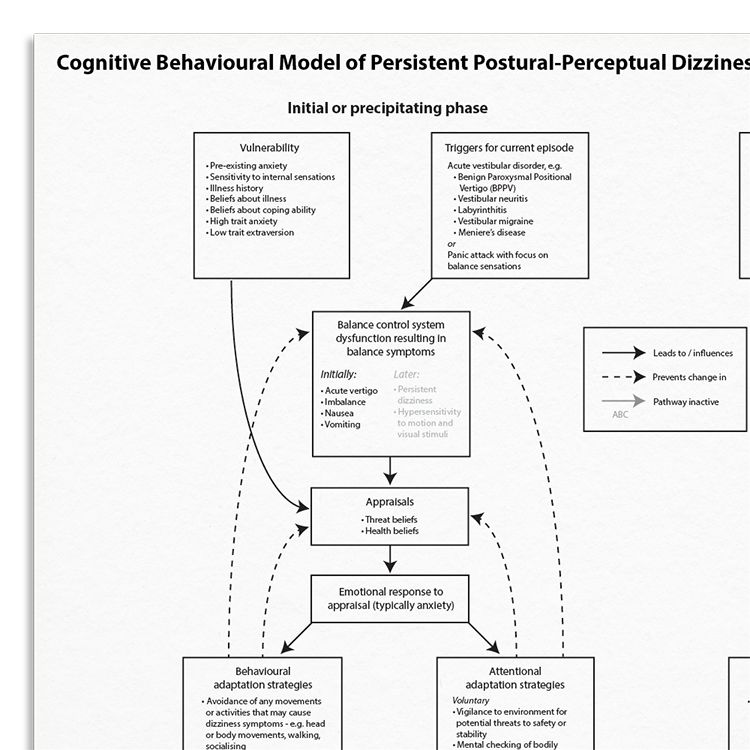
Persistent postural-perceptual dizziness (PPPD) is a chronic dizziness which is believe to be maintained, at least in part, by psychological factors. This model offers clinicians insights into the psychophysiological mechanisms responsible for the onset and persistence of dizziness. The model has parallels with health anxiety models, providing a framework for understanding PPPD presentations, and guiding targeted behavioral and cognitive interventions.
This resource serves as a useful psychological tool for practitioners managing PPPD. It provides:
Characterized by persistent dizziness and visual sensitivity.
Individuals with excessive worry about their balance and perceived physical health.
Understand more about the cognitive behavioral model of PPPD.
Use the model as a template to organize your case formulations.
Use your knowledge of the model to explain maintenance processes to clients.
Engage clients in discussions about their beliefs and behaviors.
Customize interventions based on individual maintenance mechanisms.
Use in supervision to discuss formulation and treatment plans.
Whalley and Cane’s (2017) Cognitive Behavioral Model of Persistent Postural-Perceptual Dizziness (PPPD) proposes that psychological factors play a key role in the maintenance of chronic dizziness symptoms. It suggests that the way individuals interpret and respond to sensations of dizziness can significantly influence symptom persistence. In particular, threat-based appraisals — such as viewing dizziness as a sign of serious illness or imminent danger — can trigger anxiety and physiological arousal, which in turn amplify the experience of dizziness.
Over time, individuals often develop coping strategies that unintentionally maintain or worsen their symptoms. These may include excessive monitoring of balance-related sensations, hypervigilance, avoidance of certain environments or movements, and reliance on safety behaviors such as holding onto furniture or avoiding crowds. While these strategies may feel protective in the short term, they can prevent habituation, reinforce threat interpretations, and reduce confidence in the body’s ability to self-regulate. This creates a self-perpetuating cycle in which dizziness is anticipated, monitored for, and more readily experienced.
Therapeutically, the model provides a practical framework for helping clients understand the links between their beliefs, attention, and behaviors. Treatment often involves psychoeducation about the benign nature of normal dizziness, cognitive work to challenge catastrophic appraisals, and behavioral experiments to reduce avoidance and safety behaviors. Therapists can also support clients to shift their focus away from internal monitoring and toward external engagement, which can help recalibrate attentional systems and reduce symptom intensity. The model encourages a collaborative, curious, and validating stance to support clients in regaining a sense of control and confidence in daily life.

Just enter your name and email address, and we'll send you Cognitive Behavioral Model Of Persistent Postural-Perceptual Dizziness (PPPD: Whalley, Cane, 2017) (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy