Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
Complex post-traumatic stress disorder (CPTSD) is characterized by a broad range of severe clusters following exposure to prolonged or repetitive traumatic events.

Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
To use this feature you must be signed in to an active account on the Advanced or Complete plans.
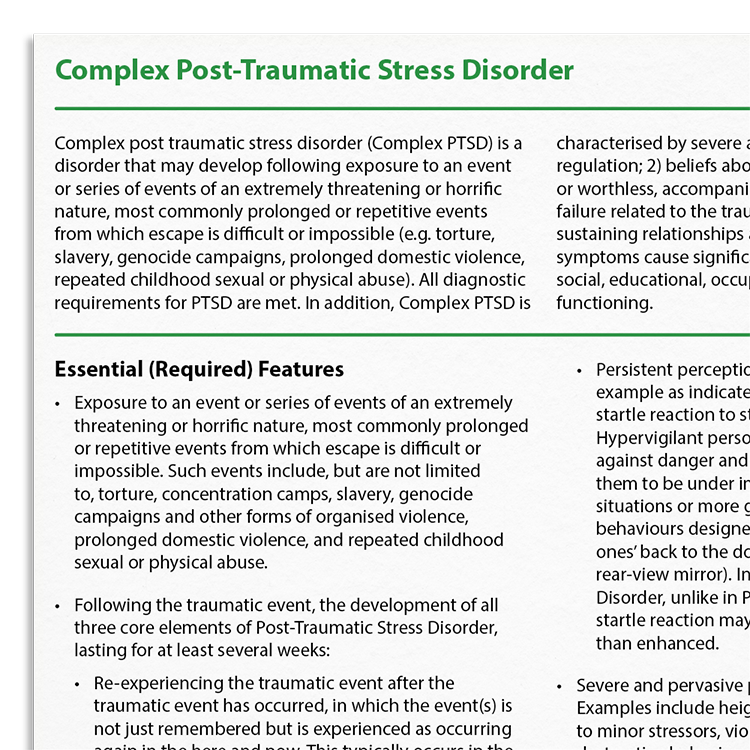
Complex PTSD develops after exposure to horrific or threatening events, such as torture or prolonged abuse, where escape is difficult. In addition to meeting diagnostic criteria for PTSD (i.e. symptoms relating to involuntary memory, hyperarousal, and avoidance), CPTSD involves severe affect regulation issues, negative self-perceptions, and relationship difficulties. These symptoms result in significantly impaired functioning across a variety of life domains.
Accurate identification of complex PTSD is crucial for effective therapeutic intervention.
Added challenges with affect regulation and a negative self-view.
Following traumatic events, meeting all core elements such as re-experiencing and avoidance.
Especially when characterised by intense emotional responses, unstable relationships, and chronic feelings of emptiness.
Identify signs of CPTSD alongside standard PTSD criteria.
Evaluate the severity of affect regulation issues and self-perception.
Develop treatment plans that consider prolonged trauma effects.
Work with clients to address challenges they face.
Adjust therapeutic techniques to manage emotional and interpersonal symptoms.
Complex PTSD extends the established PTSD framework to account for the effects of prolonged, repeated, or interpersonal trauma. While core PTSD symptoms such as re-experiencing, avoidance, and hyperarousal remain central and should be addressed using evidence-based treatments (e.g., trauma-focused CBT, prolonged exposure, EMDR), CPTSD also involves additional challenges including affect dysregulation, negative self-concept, and interpersonal difficulties.
Therapists should retain fidelity to standard PTSD protocols while incorporating additional interventions aimed at improving emotional regulation, strengthening self-identity, and developing interpersonal effectiveness. A phased or modular approach may be beneficial, particularly when clients present with high levels of instability or risk, although there is some clinical debate concerning whether this is necessary.

Just enter your name and email address, and we'll send you Recognizing Complex Post Traumatic Stress Disorder (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy