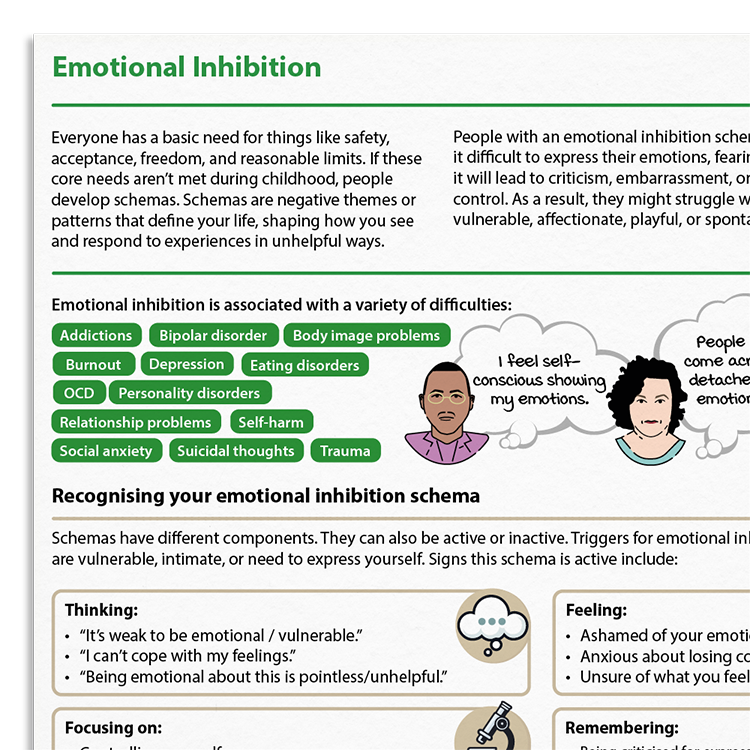
Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
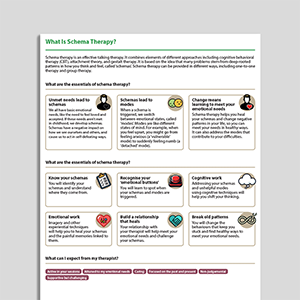
Client version
Includes client-friendly guidance. Downloads are in Fillable PDF format where appropriate.